When nicotine enters the body — whether it’s smoking a cigarette, chewing tobacco or any other method — it fires electrical signals in the body that reshape the brain at multiple levels. Examples include changing dopamine pathways, the ability to focus and basic survival instincts.
Eventually, the brain will adapt to rearranged neurological pathways, but once the nicotine wears off, the body enters the initial phase of detox, otherwise known as acute withdrawal. Scientists have found that this stage has detrimental effects on the brain, impacting sleep, attention span, heart rate, and oxygen levels.
—Lila Wollman, Principal Investigator and Assistant Professor in Department of Human Physiology
New research from College of Arts and Sciences (CAS) researchers is now suggesting that nicotine withdrawal may also affect the way we breathe. Lila Wollman, an assistant professor and researcher in CAS’s Department of Human Physiology is studying the effects of nicotine withdrawal on the body’s respiratory control.
Normally, when the body senses a low oxygen environment, it triggers a biological response to breathe harder and more frequently. Wollman hypothesizes that nicotine impacts the body’s ability to sense these changes, and as a result, those in withdrawal will not change their respiration rate.
To support her research, Wollman received a two-part grant from the National Institutes of Health designed to support post-doctorate researchers in developing independent research paths.
“The pitch for this grant is to not only show this theory has potential, but you also have potential as a scientist, so they should invest in you as a researcher,” Wollman explains. “It must be a novel idea that's different from what your mentor studies, so it's your independent research direction.”
Wollman completed the initial phase of the grant at the University of Arizona where she carried out early research in her mentor's lab under close guidance. Now at the UO, she will receive $249,000 per year in funding to continue her experiment independently until 2027.
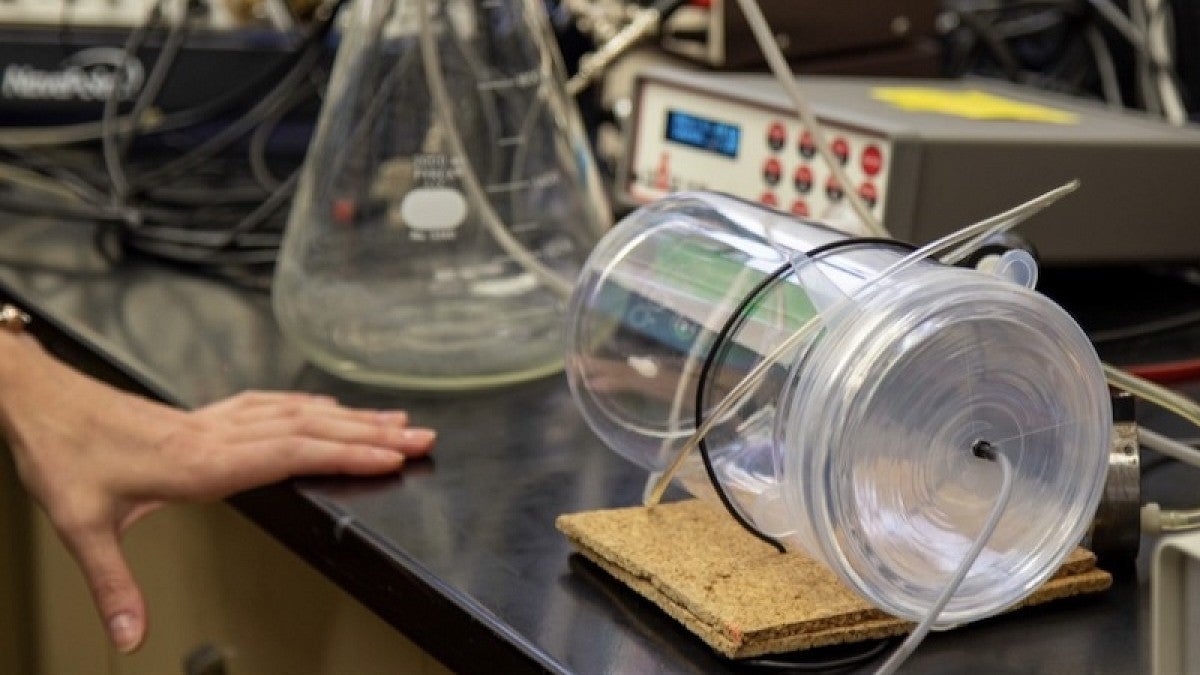
To test the effect of nicotine withdrawal on oxygen sensing, Wollman has been studying lab rats in three different groups, two of which received nicotine and one that served as the control group and didn’t receive any nicotine.
Outcomes of the research on nicotine and respiratory issues
Wollman notes her findings may have real implications for nicotine users with respiratory issues.
“If somebody who smokes enters the hospital unexpectedly due to a medical condition, they're very quickly going to be in nicotine withdrawal,” she said. “Nicotine withdrawal, which has kind of historically been thought of as uncomfortable, but not really dangerous, may be more dangerous for those already experiencing pulmonary or cardiovascular disorders. This might be something important that we should be monitoring.”
Along with this, Wollman hypothesizes that those who repeatedly try and fail to quit nicotine intake could be even more vulnerable to certain respiratory functions.
Studying other effects of nicotine
While Wollman’s research is set to run through 2027, her goal is to find new avenues from this topic. Beyond breathing, Wollman is beginning to ask how nicotine withdrawal during sleep might ripple into long-term health effects like Alzheimer's.
“Since nicotine is so rapidly metabolized, when people who use nicotine throughout the day go to sleep, they are spending most of the night in nicotine withdrawal,” she said. “I've become interested in how, if every night during sleep, they're not breathing as well, how is that potentially contributing to long-term disease outcomes?”
She is currently working on a grant to continue her research in this direction with Ashley Walker, a human physiology researcher in CAS and an expert in the involvement of the cardiovascular system in cognitive diseases like Alzheimer’s. Walker has been her biggest mentor for this upcoming project.
“Although studying Alzheimer’s is not in my field even remotely, Ashley has helped me both with the intellectual material and the techniques involved,” Wollman said. “She’s really been helping me out, and she's one of my co-investigators on this grant.”
If Wollman’s theories hold true, it could change the way scientists and clinicians think about the risks of nicotine dependence.
—By Leo Brown, College of Arts and Sciences
